|
 |
- Search
| J Korean Crit Care Nurs > Volume 14(3); 2021 > Article |
|
ABSTRACT
Purpose
This systematic review was conducted to identify which dyadic intervention could be implemented for heart failure patient–family caregiver dyads to improve patient and/or their family caregivers outcomes.
Methods
Eleven databases were searched from their inception to July, 2021. This review considered any randomized controlled trials that evaluated the effectiveness of intervention including heart failure patient-family caregiver dyads. Two reviewers independently evaluated the methodological quality using the Cochrane Collaboration's tool for assessing risk of bias and extracted details of the included studies. The studies included in this review were not suitable for metaanalysis and therefore the results were presented as a narrative summary.
Results
Six studies including 900 dyads were included and mainly primary family caregiver of patients was spouse. Majority of dyadic intervention were focused on psychoeducational intervention excepting one study on mobile health intervention. All studies included in this review focused on patients’ outcomes compared to family caregivers’ outcomes and dyadic outcomes. Individual interventions improved quality of life among heart failure patients and their family caregivers in two articles. The overall quality of selected articles was low.
Conclusion
This study provides moderate support for the use of a dyadic intervention to improve quality of life among heart failure patients and their family caregivers. More rigorous high-quality studies investigating interventions to meet the needs of patient and family caregivers in heart failure care are needed.
심부전(heart failure, HF)은 심장의 구조적 또는 기능적 이상으로 인한 심장의 펌프기능 장애로서, 심장이 더 이상 효율적으로 혈액을 내보낼 수 없을 때 발생하는 만성 진행성 임상증후군을 의미한다[1]. 심부전은 호흡곤란과 부종 등의 증상을 주호소로 악화와 완화를 반복하는 특징을 갖고 있으며[2], 국내 심부전 유병률은 2019년 기준 14만 2천명으로 2009년 9만 4천명에 비해 지속적으로 높아지고 있다[3]. 심부전으로 인한 30일 이내 재입원율은 약 20%, 1년 이내 사망률은 약 17∼45%로서[4,5] 예후가 나쁜 중증 질환으로 인식되고 있다. 특히 심부전은 노인성 질환이라고 불릴만큼 노인에서의 유병률이 높을 뿐 아니라 갑작스런 증상악화로 인한 잦은 재입원 및 장기간의 질환관리가 요구되므로, 환자 개인뿐 아니라 국가차원의 의료비 부담이 가중되고 있어[6] 적극적인 관심과 다각적인 대책이 요구된다.
심부전은 질환 특성상 완치가 어렵기 때문에 처방약의 정확한 복용과 더불어 영양관리, 적절한 운동, 규칙적인 증상 모니터링 등과 같은 포괄적 생활습관 개선이 중요하며, 이를 위한 지속적인 자가간호가 요구된다[7]. 2016년 European Society of Cardiology (ESC) 가이드라인에서도 생활습관 교정을 위한 자가간호가 심부전 환자의 사망률을 낮추고, 삶의 질을 개선하는데 중요 요소라고 하였다[1,8]. 특히 노인 심부전 환자의 경우, 고령으로 인한 일상생활능력 감소와 인지기능 저하 및 복합 만성질환을 동반하는 경우가 많다[4,6]. 이러한 특징은 심부전 환자로 하여금 약물복용을 포함한 자가간호와 치료관련 의사결정 등에 부정적 영향을 미치게 되며[9], 이로 인해 심부전 환자는 질환관리 내용 중 상당한 부분을 가족 돌봄제공자에게 의지하는 경우가 많다[10]. 선행연구에 따르면, 심부전 환자의 가족 돌봄제공자는 평균 주 22시간을 심부전 환자의 일상생활, 자가간호 유지 및 관리, 외래 방문 시 동반자 역할 등을 수행하는 데 보내고 있으며[11], 심부전 환자간호에 참여하는 가족 돌봄제공자는 피로, 수면장애, 불안, 우울과 같은 신체적·정신적 건강문제는 물론 경제적 부담까지 감당하게 된다고 알려져 있다[12,13]. 이와 같은 가족 돌봄제공자의 어려움은 결국, 심부전 환자의 건강상태 및 예후에 부정적 영향을 미치게 되어 악순환을 야기한다[11,13]. 지금까지 수행된 심부전 환자 또는 가족 대상의 중재연구를 살펴보면, 심부전 환자만을 대상으로 한 자가간호 역량 강화 중재 프로그램 적용 후 심부전 환자의 재입원율, 사망률 감소 및 삶의 질 개선 효과를 보였으며[14], 심부전 환자의 가족 돌봄제공자를 대상으로 한 상담프로그램 중재 적용 후 심부전 환자의 재입원률 감소, 주 돌봄 제공자의 우울 정도가 감소하였다는 보고가 있었다[15]. 그러나 이들 환자 또는 가족 대상 중재연구들은 장기간의 긍정적 또는 유의한 효과는 나타나지 않았다[16]. 이에 최근 심부전 환자와 가족 돌봄제공자를 함께 고려한 다이애딕 중재프로그램 개발 및 적용이 시도되기 시작하였다[13].
다이애드(dyad)란 사회학적으로 의미있는 관계를 유지하는 두 개인을 지칭하는 용어로, 심부전 환자와 가족 돌봄제공자를 하나의 다이애드로 지칭할 수 있다[16]. 최근 뇌졸중, 치매 환자와 가족 돌봄제공자를 대상으로 한 다이애딕 중재프로그램 적용 후 환자와 가족 돌봄제공자의 신체적, 심리적, 정신적 측면의 긍정적 개선효과는 물론, 가족 돌봄제공자의 간호부담감 완화에 기여한다는 연구결과가 보고되면서[17–19], 심부전 환자와 가족 대상의 다이애딕 중재연구들이 증가하기 시작하였다[9]. 지금까지 수행된 심부전 환자와 가족 돌봄제공자를 위한 다이애딕 중재에 관한 체계적 고찰 연구는 단 한편으로[16], 심부전 환자와 가족 돌봄 제공자에게 시행된 다이애딕 중재의 종류 및 구성요소를 단순히 소개하는 데 그치고 있다. 따라서, 본 연구는 심부전 환자와 가족 돌봄제공자를 대상으로 수행된 다이애딕 중재관련 무작위 대조군 실험연구들을 체계적으로 고찰하므로 써, 중재내용 및 중재효과를 살펴보고, 향후 심부전 환자와 가족 돌봄제공자의 건강결과를 향상시킬 수 있는 환자-가족 중심 다이애딕 중재개발 연구의 방향성을 제시하고자 시도되었다.
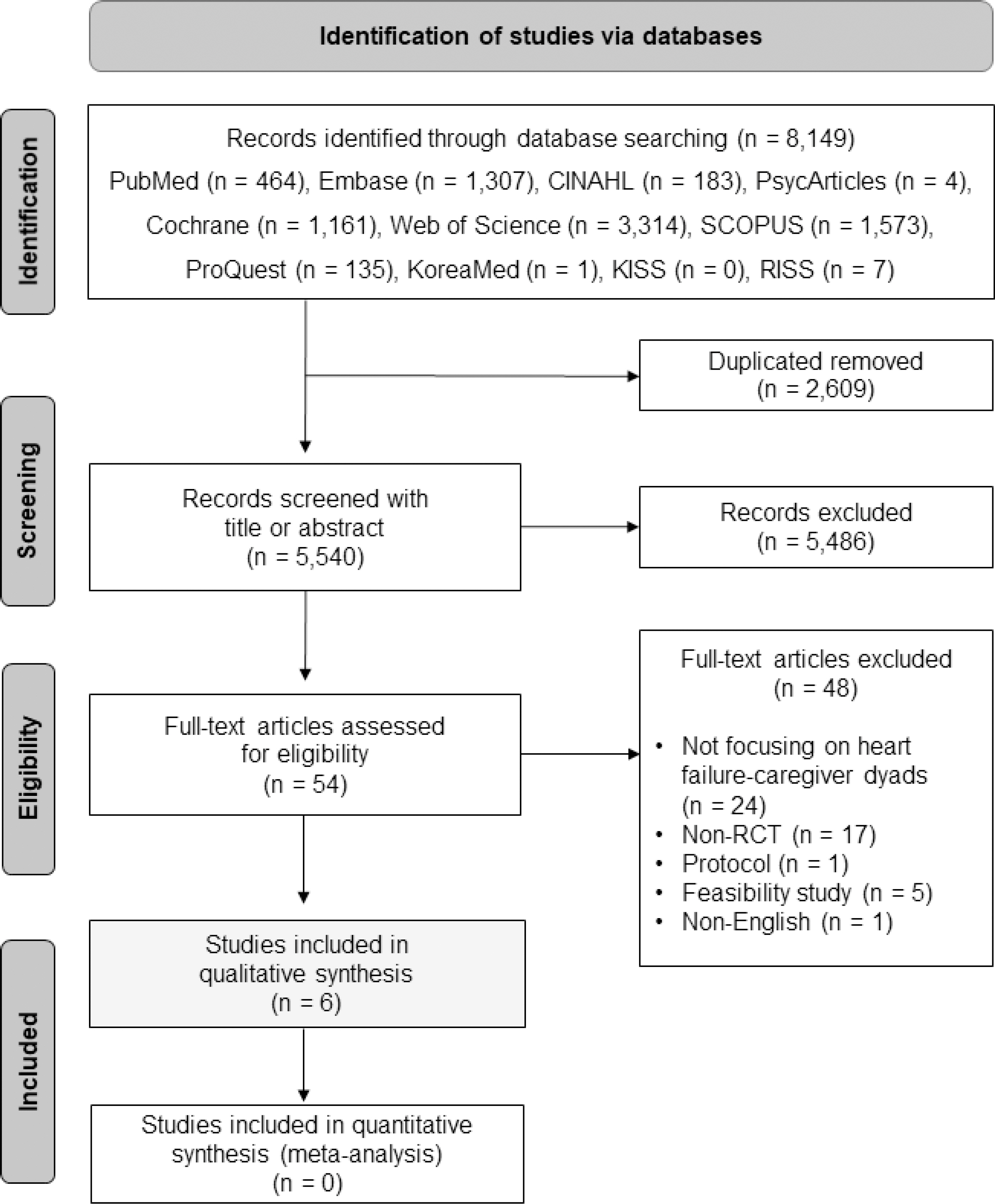
본 연구는 심부전 환자와 가족 돌봄제공자 대상의 다이애딕 중재를 실시한 연구의 특성과 중재효과를 확인하기 위한 체계적 고찰연구로서, 문헌검색 및 선정과정은 Preferred Reporting Items for Systematic review and Metaanalysis (PRISMA) Checklist [20]에 따라 이루어졌다. 본 연구의 프로토콜은 체계적 고찰 수행에 앞서 International Prospective Register of Systematic Reviews (registration number: CRD42021270522)에 등록되었다.
분석대상 문헌의 선정기준은 PICO-SD (Participants (P), Intervention (I), Comparison (C), Outcome (O), Study design (SD)) 형식에 따라 연구대상자(P)는 심부전 환자와 가족 돌봄제공자, 중재(I)는 다이애딕 중재프로그램, 비교 중재(C)는 다이애딕 중재프그램을 적용하지 않은 군, 결과(O)는 환자 또는 가족 돌봄제공자관련 중재효과와 다이애딕 중재효과를 보고한 연구, 그리고 연구설계(SD)는 무작위 대조군 실험연구(randomized controlled trial, RCT)만을 포함하였다. 이외에도 언어는 한글과 영어로 출판된 원문으로 하였으며, 동일 중재프로그램을 사용하였으나, 중재기간과 결과변수를 달리 적용한 경우는 포함하였다. 단, 체계적 고찰, 프로토콜, 유용성 연구, 질적연구, 관찰연구, 초록, 학술대회 발표자료 등은 제외하였다.
문헌 검색을 위한 국내 데이터베이스는 KoreaMed, 한국학술정보(KISS)와 한국교육학술정보원(RISS)을 이용하였고, 국외 데이터베이스는 PubMed, EMBASE, CINAHL, PsycArticles, Cochrane Library, Web of Science, Scopus, ProQuest를 사용하였다. 문헌검색 기간은 각 데이터베이스의 검색가능한 시작년도로부터 2021년 7월 30일까지로 하였다. 검색어는 학술지의 제목, 초록, 키워드로 제한하여 국내의 경우 (‘심부전’) AND (‘가족’) AND (‘중재’ OR ‘프로그램’)으로 실시하였으며, 국외의 경우 (‘heart failure’ OR ‘ventricular dysfunction’ OR ‘cardiomyopathy’) AND (‘dyad’ OR ‘caregiver’ OR ‘carer’ OR ‘partner’ OR ‘couple’ OR ‘family’ OR ‘spouse’) AND (‘intervention’ OR ‘program’ OR ‘experimental’ OR ‘RCT’)를 사용하여 문헌을 검색하였다.
문헌검색 결과, 국내⋅외 데이터베이스로부터 총 8,149편의 문헌이 추출되었으며, 검색된 문헌들은 서지관리 프로그램(EndNote 20)을 이용하여 검토 및 정리하였다. 중복문헌을 제거한 후 총 5,540편의 문헌을 대상으로 문헌의 선정기준과 제외기준에 따라 연구 제목과 초록을 확인하여 연구대상으로 적합한 54개의 문헌을 선별하였다. 이후 문헌의 전문(full-text) 검토를 통해 심부전 환자와 가족 돌봄제공자를 하나의 단위로 연구대상자에 포함한 연구가 아닌 24편, 무작위 대조군 실험연구가 아닌 17편, 프로토콜 1편, 프로그램의 유용성 평가 5편, 한글 또는 영어가 아닌 1편을 제외한 최종 6편의 문헌이 분석대상으로 선정되었다(Figure 1). 문헌 선정과정은 두 명의 연구자가 독립적으로 수행하여 이루어진 검색결과에 대해 연구자 간 이견이 있을 경우 충분한 논의를 통해 합의를 이루는 방식으로 진행하였다.
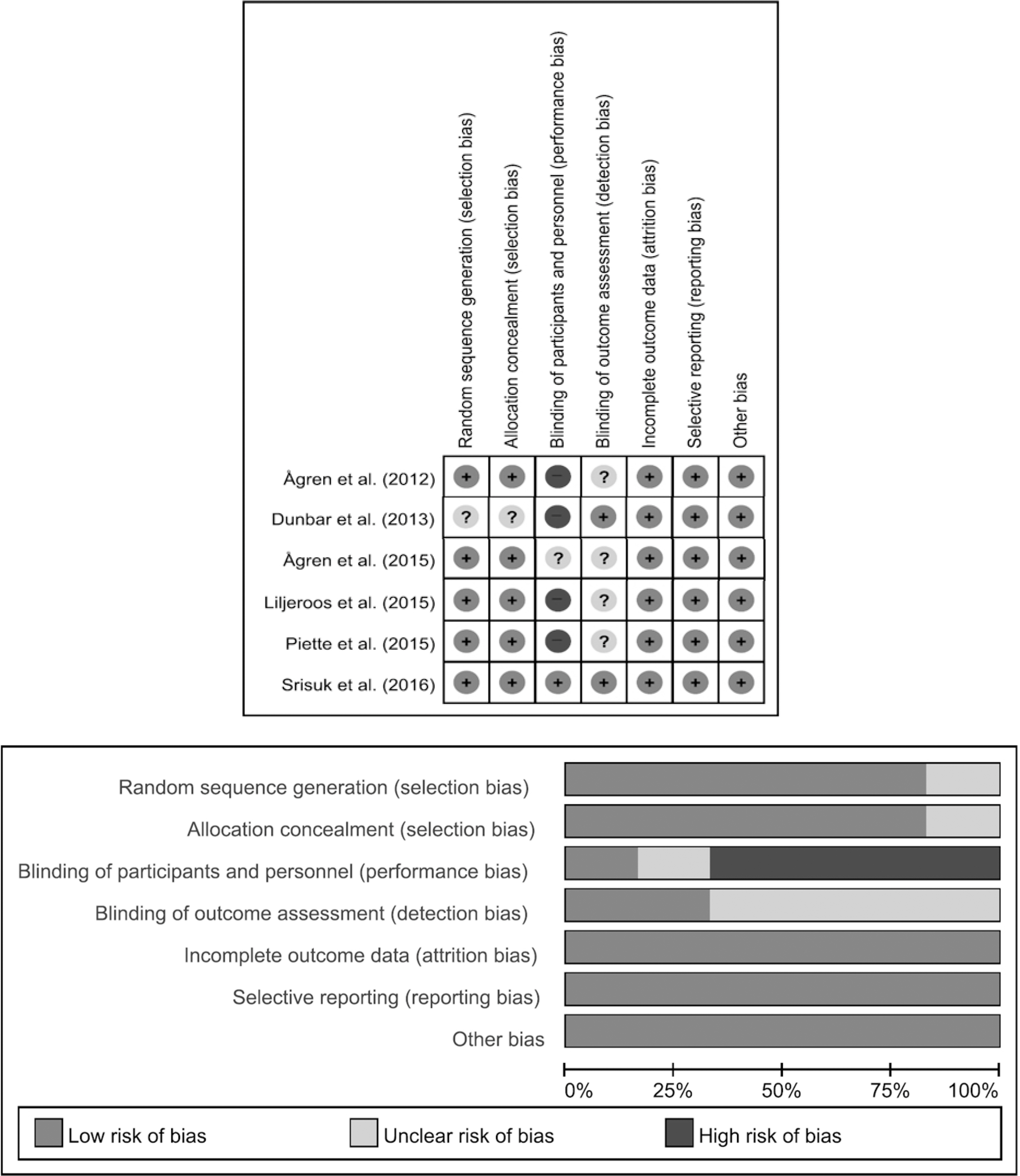
선정된 6편의 문헌의 질평가는 코크란 연합의 The Cochrane's Risk of Bias (RoB)를 사용하였다[21]. RoB는 무작위 배정순서 생성, 배정순서 은폐, 대상자 및 연구자의 눈가림, 결과평가자 눈가림, 불완전한 결과의 처리, 선택적 결과 보고, 타당도를 위협하는 다른 잠재적 비뚤림 위험(이해상충, 시험비 지원기관, 잠재적 비뚤림 등)의 총 7문항에 대해 비뚤림 위험이 ‘낮음’, ‘높음’, ‘불확실’로 평가할 수 있도록 구성되어 있다. 독립된 두 명의 연구자가 각각 질 평가를 실행한 후 일치 여부를 검토하여 최종 비뚤림 위험 결과를 판정하였다. 일치되는 않는 사항에 대해서는 충분한 논의를 거친 후 합의를 거쳤다.
분석대상 논문에 대한 분석은 Microsoft Excel 2016 프로그램을 사용하여 저자, 출판연도, 출판국가, 연구 설계, 대상자(연령, 성별, The New York Heart Association Functional classification (NYHA), 주 돌봄제공자 유형), 중재 방법(중재 종류, 내용, 기간), 측정 변수 및 측정 도구, 측정 시기, 주요 결과로 자료 추출 항목을 구성하였다. 이후 분석대상 문헌을 출판연도 순으로 배열한 후, 자료의 정확성 확보를 위해 두 명의 연구자가 독립적으로 자료 추출을 시행하였다. 추출 후 세 번째 연구자가 두 명이 추출한 자료를 다시 검토 후 최종 분석대상 논문을 확인하였다. 본 연구에서 비뚤림 평가는 RevMan 5.3프로그램을 이용하였다. 본 연구의 체계적 고찰에 포함된 6편의 무작위 대조군 실험연구는 각 연구의 이질적인 특성으로 인해 중재 방법의 효과크기를 결정할 수 없어 메타분석을 실시할 수 없었다.
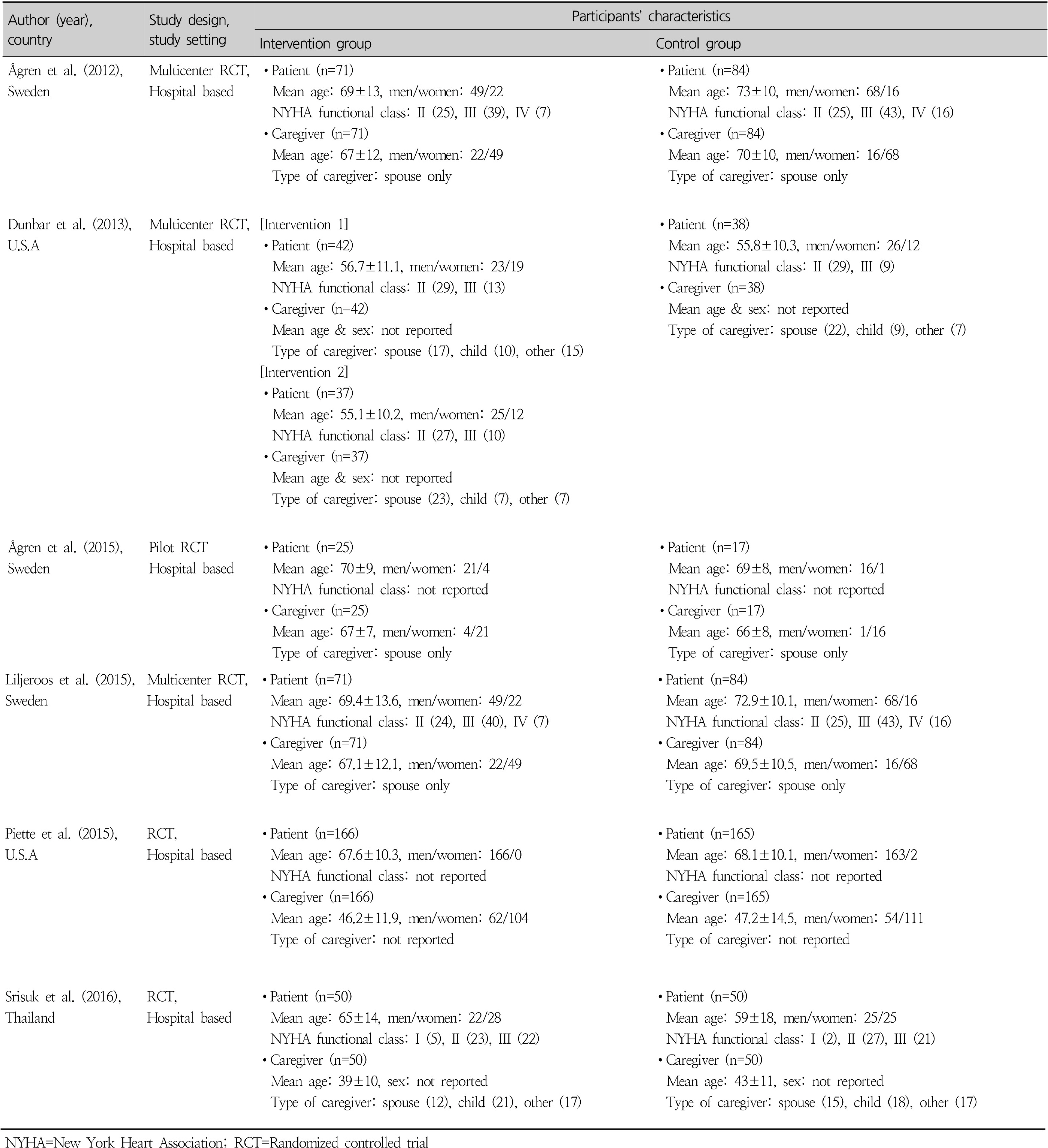
심부전 환자와 가족 돌봄제공자 대상의 다이애딕 중재에 최종 분석된 논문은 총 6편으로[9,10,23–26], 출판연도는 2012년부터 게재되었으며 국가는 스웨덴 3편[10,23,25], 미국 2편[24,26], 태국 1편[9]이었다(Table 1). 분석대상 6편 모두 병원 기반 연구였다. 연구대상자 수는 총 900쌍으로 50쌍 미만의 논문은 2편[24,25], 50쌍 이상에서 100쌍 미만의 논문은 3편[9,10,23], 100쌍 이상의 논문은 1편[26]이었다. 심부전 환자의 평균 연령은 실험군과 대조군 모두 평균 65세 이상인 논문이 4편[10,23,25,26]으로 가장 많았으며, 심장 중증도 기능분류인 NYHA class는 4편만 보고되었는데[9,10,23,24]Ⅰ단계에서 Ⅳ단계까지 다양하게 나타났다. 심부전 환자 가족의 평균 연령은 심부전 환자와 유사하게 실험군과 대조군 모두 65세 이상인 논문이 3편[9,23,25]이었고, 가족 돌봄제공자의 유형으로 배우자로만 한정된 논문은 3편이었다[10,23,25].
RoB 도구의 7가지 평가항목에 따라 항목별 비뚤림 위험성은 불완전한 결과 처리, 선택적 결과 보고, 타당도를 위협하는 다른 잠재적 비뚤림 위험 3가지 항목에서 6편(100%) 모두 낮은 비뚤림으로 평가되었다. 반면, 대상자와 연구자의 눈가림은 4편(66.7%)은 고위험으로 평가되었고[10,23,24,26], 결과평가자 눈가림 4편(66.7%)은 불확실로 분류되었다[10,23,25,26].
다음으로 중재프로그램 보고의 질 평가결과(Table 2), 중재 설계와 내용과 관련된 총 9가지 항목 모두를 충족한 논문은 1편[26]에 불과하였다. 특히, 중재전달방법에 대한 기술 항목이 누락된 문헌은 5편[9,10,23–25]으로 가장 많았고, 다음은 중재의 각 세션별 내용을 상세하게 기술하지 않은 논문이 3편[9,10,23]으로 나타났다.
Completeness of Intervention Reporting
선택된 문헌의 중재 특성은 Table 3에 제시하였다. 중재 종류는 심리사회적 교육프로그램 5편[9,10,23–25], 모바일 프로그램 1편[26]이었으며, 중재 기간은 최소 3개월부터 최대 8개월로 나타났다. 중재 후 다이애딕 측면의 중재효과 결과변수로는 삶의 질, 우울, 지각된 자아조절(perceived control), 심부전 지식이 포함되었으며, 환자와 가족 돌봄제공자 각각의 중재효과 결과변수로는 환자의 경우, 삶의 질, 우울, 자가간호, 심부전 지식, 약물복용 이행, 지각된 자율성지지(patient perceived autonomy support), 지각된 가족 평가(perceived family criticism), 의사소통 강도(communication intensity)가 측정되었으며, 가족 돌봄제공자의 경우, 삶의 질, 간호부담감, 가족 돌봄제공자의 지각된 자아조절이 측정되었다. 이 중 중재효과의 결과변수로서 삶의 질을 활용한 논문이 5편으로[9,10,23,25,26], 가장 많았으며, SF-36을 이용한 삶의 질 측정이 3편[10,23,25]이었고, 중재적용 후 환자와 가족 모두 삶의 질이 개선된 논문은 2편[9,25]으로 나타났다. 삶의 질 다음으로는 우울을 측정한 논문이 3편[10,23,25]이었으나, 3편 모두 실험군과 중재군에 참여한 환자와 가족 돌봄제공자의 우울은 통계적으로 유의하지 않았다.
심부전 환자의 성공적인 자가간호를 위해서는 단순히 심부전 환자교육에만 초점을 두는 것에서 벗어나, 일상생활에서 서로 밀접한 관계를 맺고 있는 가족 돌봄제공자의 참여를 함께 고려한 중재전략이 중요하겠다[27,28]. 이에 본 연구는 심부전 환자와 가족 돌봄제공자를 대상으로 시행된 다이애딕 중재 프로그램의 특성과 효과를 체계적으로 고찰한 연구를 시도하였다.
먼저 본 체계적 고찰연구에 포함된 분석대상 논문의 일반적 특성을 살펴보면, 분석대상 6편 모두 병원기반 다이애딕 중재연구들이었다. 이는 의료진이 단순히 심부전 환자의 증상관리에만 초점을 두지 않고 환자의 치료 또는 예후에 영향을 미치는 가족 돌봄제공자도 함께 고려한 질환관리가 중요함을 인지하고 있다고 할 수 있다[12]. 그러나 태국에서 수행된 1편[9]을 제외한 5편은 모두 유럽과 북미를 중심으로 시행되어져, 다이애딕 중재의 실제적 효과와 효과적인 프로그램 구성을 위해서는 국내는 물론 다양한 국가에서 심부전 환자와 가족 돌봄제공자 대상의 다이애딕 중재가 개발될 필요가 있겠다. 본 체계적 고찰에 포함된 다이애딕 중재연구에 참여한 대상자의 평균 연령은 65세 이상이 6편 중 4편으로 가장 많았고[9,10,23,25], NYHA 기능적 분류를 보고한 4편 모두 Ⅱ-Ⅲ 단계의 대상자가 가장 많이 포함되었다[9,10,23,24]. 이는 65세 이상의 노인 심부전환자의 인지기능 수준이 낮을수록 자가관리 이행이 떨어지고 부정적인 건강 결과를 야기하므로[29,30] 노인 심부전 환자와 가족을 대상으로 다이애딕 중재와 NYHA Ⅱ-Ⅲ 단계의 자가간호가 중요한 그룹[31]에서 다이애딕 중재연구가 많이 시도되고 있음을 유추할 수 있다. 특히 NYHA 중증도 분류단계가 높을수록 적절한 자가간호가 이루어지지 않을 경우 재입원과 사망률이 높고[31], 인지적 또는 신체적 기능 저하로 인해 환자 개인만의 노력만으로 효과적인 건강관리를 유지하는 데 제한이 있으므로[32], 심부전 환자의 질환관리에 대한 긍정적인 인식과 생활습관 개선을 위해서는 가족 구성원의 적극적인 참여를 바탕으로 한 보다 많은 수의 다이애딕 중재 연구가 시행될 필요가 있다. 또한 가족 돌봄제공자의 유형을 살펴보면, 배우자가 가장 많았고 배우자로 한정된 다이애딕 중재 또한 3편[10,23,25]으로, 이들 배우자의 평균 연령은 67세로 나타났다. 국내 심부전 환자 대상 연구들에 의하면 배우자가 있는 심부전 환자의 경우 독거 환자나 배우자 이외의 동거가족이 있는 환자에 비해 자가간호 이행률이 높다고 보고하였다[33,34]. 이는 심부전 환자 치료계획 수립 시, 배우자가 있는 심부전 환자의 경우, 배우자를 적극적으로 치료관련 의사결정에 참여할 수 있도록 하는 방안이 필요함을 시사한다. 그러나, 본 연구결과 심부전 환자의 배우자 또한 주로 고령임을 감안할 때, 의료진들은 노인 부부 중심의 맞춤형 다이애딕 중재를 우선적으로 고려할 필요가 있겠다. 한편, 가족 돌봄제공자가 자녀인 경우와 친척 및 지인인 관계로 보고한 2편[9,26]의 논문에서는 연구에 참여한 대상자 수가 7명에서 21명이었고 평균 연령 범위도 39세에서 46세로 상대적으로 젊으므로, 노인 부부 중심의 다이애딕 중재와 다른 결과가 나타날 수 있다. 따라서, 향후 가족형태나 돌봄제공자의 연령층을 고려한 다양한 가족특성을 고려한 다이애딕 중재연구들을 시도할 필요가 있다. 나아가 환자와 가족 모두의 건강상태와 삶의 질을 향상시키기 위한 목적의 다이애딕 중재를 계획한다면, 가족 돌봄제공자의 범주를 단순 혈연관계나 현재 함께 거주하고 있다는 사실만으로 한정하지 말고, 장기간에 걸친 환자의 질환관리에 지속적인 관심을 가지고, 주된 돌봄역할을 하는 대상자가 누구인 지를 파악하는 것이 연구수행 전 면밀한 고려가 요구된다.다음으로 본 연구에 포함된 분석대상 논문들의 문헌의 질을 평가한 결과, 연구자와 대상자인 환자와 가족 돌봄제공자에 대한 눈가림이 1편[9]을 제외한 나머지 5편[10,23–26]의 논문에서 이루어지지 않았고 환자와 가족 돌봄제공자의 결과평가에 대한 눈가림 또한 4편[10,23,25,26]이 불확실한 것으로 나타났다. 심부전 환자와 가족 돌봄제공자를 대상으로 이루어지는 다이애딕 중재는 교육과 심리적 지지가 중재내용의 주를 이루는 특성상 연구 대상자와 연구자를 철저하게 눈가림을 시행하고 환자 결과를 평가 시에도 눈가림을 시도하는 것은 현실적으로 어려움이 있다고 보여진다. 다음으로 다이애닉 중재프로그램의 보고에 대한 질을 평가한 결과, 중재를 적용한 연구장소에 대한 기술은 6편 모두 충실히 보고하고 있었다. 그러나, 중재 적용시 활용된 자원이나 개발과정에 대한 기술이 부족하거나[9,23] 각 중재 세션별 실시한 중재내용을 구체적으로 보고하지 않은 논문도 3편[9,10,23]으로 나타났다. 특히 중재 프로그램 적용방법에 대한 기술 측면에서 1편[26]을 제외한 5편 모두 보고내용이 불충분한 것으로 확인되었다. 따라서 향후 다이애딕 중재프로그램 개발 시 프로그램의 설계과정과 적용단계별 상세 내용을 기술하여 다양한 인구사회학적 배경과 질병관련 특성을 가진 심부전 환자와 가족 돌봄제공자 참여 프로그램을 적용할 수 있도록 관련 의료진들과 연구자 간 긴밀한 협조가 필요하겠다.본 연구의 주요 연구목적인 심부전 환자와 가족 돌봄제공자를 위한 다이애딕 중재 프로그램 내용과 효과를 살펴본과, 본 연구에 최종 선정된 6편의 다이애딕 중재 프로그램은 간호사 주도 심리교육 중재, 환자-가족 교육프로그램, 가족 파트너십 중재, 심리교육지지 중재, 모바일 건강 서비스 중재, 가족참여 교육프로그램으로 다양한 명칭으로 표현되고 있었다. 그러나 분석된 문헌들은 교육 중재[9,10,24]와 면대면과 전화를 활용한 상담 중심의 심리지지 중재[9,10,23–25] 또는 소책자, DVD, CD-ROM, 자동음성장치 등의 전달매체를 중심[9,10,23,24,26]으로 활용하였다. 또한 분석 대상 논문에 포함된 다이애딕 중재프로그램들은 대개 심부전 증상과 관련된 모니터링, 생활 개선을 위한 자가간호 내용 뿐 아니라 환자와 가족 돌봄제공자 간의 상대방에 대한 인식과 관계성 향상에 관한 내용까지 포함하고 있었다. 특히 선정된 다이애딕 중재 내용 구성은 심부전 환자의 건강상태와 요구도를 우선적으로 고려하여 교육이 6편 모두에 포함되었고, 중재의 전달 방식은 일대일 대면 상담과 전화 상담, 소식지와 소책자 및 DVD와 같은 교육자료, 컴퓨터나 모바일, 이메일 등 다양한 방법들이 활용되고 있었다. 분석대상 6편 중 1편[26]만이 모바일 기기를 활용한 다이애딕 중재를 적용하였는데, 심부전 환자 가족에게 환자관련 내용을 매주 상호 피드백하고, 위험 증상이 있을 때는 팩스 둥울 이용해 의료진과 상호협력하는 프로그램을 수행하여, 환자와 가족 모두의 삶의 질 개선에는 통계적 유의한 결과를 보이지않았으나, 중재 후 6개월과 12개월째의 규칙적인 약물복용률은 대조군에 비해 통계적으로 유의하게 높게 나타났다. 기존 선행연구들에 의하면 모바일이나 태블릿 PC 등의 다양한 디지털 기기들을 적절히 활용하는 다이애딕 중재들은 환자와 가족의 건강상태와 변화를 입력하고 모니터링하고 위험 증상시 적절한 피드백을 받는데 활용될 수 있는 장점이 있다[35,36]. 따라서 심부전 환자-가족 대상 다이애딕 중재 프로그램 시 모바일 기기 또는 원격모니터링을 활용한 프로그램도 시도할 필요가 있다. 한편, 선정된 논문에서 다이애딕 중재 효과를 확인하기 위한 종속변수는 환자와 가족 돌봄 제공자의 지각된 자아조절, 심부전 지식, 우울, 자가간호 이행, 약물복용 이행, 의사소통, 삶의 질 등 다양한 변인들이 활용되었다. 삶의 질을 결과변수로 중재효과를 살펴본 논문 5편[9,10,23,25,26]에서 2편[9,25]의 연구에서 다이애딕 중재프로그램으로 환자와 가족 삶의 질
개선에 효과가 있었음을 보고하였는데, 이 두 논문에서 개별적인 면대면 교육을 6개월 이상으로 설계한 공통점이 발견되었고 심리교육 중재는 특히 정서적 지지 차원에서 중재효과가 있음이 확인되었다. 이러한 결과를 바탕으로, 심부전 환자와 가족 돌봄제공자 참여 다이애딕 중재 개발시 중재 기간과 구성내용 및 중재 전달 방식에 대한 신중한 고려 뿐만아니라, 심부전 환자와 가족 돌봄제공자 모두의 신체적, 정신적 건강상태를 증진키실 수 있도록 다이애딕 중재목표를 설정하여, 심리사회적 결과변수 뿐 아니라 객관적인 임상검사 결과 등도 적극 활용하여 중재효과를 측정하는 것이 필요함을 알 수 있다. 본 체계적 고찰 결과, 분석대상 논문의 과반수 이상이 환자측면의 결과변수에만 초점을 두고 있고[24–26] 가족 돌봄제공자 관련 결과변수 혹은 환자-가족을 함께 측정한 다이애딕 결과변수들은 상대적으로 부족하였다. 이는 심부전 가족 돌봄제공자 또는 환자-가족 다이애딕 변수를 측정할만한 표준화된 도구가 부족한 것과 관련있다. 따라서 심부전 환자와 가족 돌봄제공자 대상 다이애딕 중재프로그램 적용시 중재효과를 측정할 수 있는 신뢰도와 타당도가 확보된 도구개발이 요구된다. 또한, 심부전 환자와 가족 돌봄제공자 모두에게 적용할 수 있는 측정도구가 개발된다면, 환자와 가족 돌봄제공자 간 상호작용 효과나 메타분석 결과를 도출하는 데 유용할 것이다.
본 체계적 고찰연구는 한글과 영어로만 된 논문만을분석대상으로 하였으며, 심부전 환자와 가족 돌봄제공자를 하나의 단위로 간주한 다이애딕 중재연구만을 포함하였다는 제한점이 있다. 본 연구를 통해 다이애딕 중재연구의 효과를 일반화하기에는 논문의 편수가 부족할 뿐 아니라 분석 논문들 간의 이질성이 높아 지속적인 연구결과가 축적된 후에 다이애딕 중재효과를 검증할 필요가 있겠다. 이러한 제한점에도 불구하고, 본 연구를 통해 심부전과 같은 만성질환의 경우 환자중심 또는 가족참여와 같은 개별접근이 아닌 환자와 주 돌봄제공자를 하나의 간호단위로 간주하는 다이애딕 접근이 만성질환을 가진 환자와 가족 모두의 삶의 질 증진에 기여할 수 있는 가능성을 시사하였다. 이에 보건의료전문가들은 중·장기적 만성질환자 관리를 계획함에 있어 환자와 가족 돌봄제공자를 함께 고려하여 효과적인 병원기반의 퇴원교육과 지역사회 연계형의 만성질환 관리 방안을 다각적으로 마련할 필요가 있겠다.
본 체계적 고찰 결과, 2012년 이후 병원기반의 심부전 환자와 가족 돌봄제공자 대상 다이애딕 중재연구가 이루어지고 있었으나 6편에 불과하여, 대규모의 다기관 무작위 대조군 실험연구가 필요함을 알 수 있었다. 심부전 환자와 가족 돌봄제공자 대상 다이애딕 중재에 참여한 연구대상자의 평균 연령은 65세 이상이 4편, 가족 돌봄제공자의 경우 배우자로 한정한 논문은 3편, 심부전 환자의 중증도를 반영하는 NYHA 기능적 분류는 Ⅱ-Ⅲ 단계에 해당하는 대상자가 4편으로 가장 많았다. 다이애딕 중재프로그램의 적용 기간은 최소 3개월부터 최대 8개월로 다양하였으며, 중재유형은 5편이 심리사회적 교육중재에 해당하였고 1편이 모바일 기반 다이애딕 중재였다. 분석대상 논문별 중재효과를 측정하는 변인으로 삶의 질이 가장 많이 적용되었고, 삶의 질의 경우 2편의 연구에서 다이애딕 중재프로그램 적용 후 환자와 가족 모두 삶의 질 개선 효과가 있었음을 보고하였다. 그러나, 분석대상 논문 모두 다양한 결과변수와 측정도구를 사용하고 있어 메타분석을 실시할 수 없었으며, 다이애딕 중재효과로 환자측면의 결과는 6편이었던 반면, 가족 돌봄제공자 측면과 환자와 가족돌봄제공자 간의 다이애딕 측면의 결과보고는 소수에 불과하였다. 향후 많은 수의 다이애드를 포함한 다기관, 다국적의 심부전 환자-가족 돌봄제공자 참여 다이애딕 중재연구가 시도될 필요가 있으며, 다이애딕 중재효과를 측정할 수 있는 표준화된 도구개발 및 디지털 의료환경을 반영한 하이브리드 형태의 심리사회 교육중재 프로그램 등의 개발이 요구된다.
REFERENCES
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. European Journal of Heart Failure. 2016). 18(8):891–975. https://doi.org/10.1002/ejhf.592.



Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Colvin MM, et al. 2016 ACC/AHA/HFSA focused update on new pharmacological therapy for heart failure: an update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines and the heart failure society of America. Journal of the American College of Cardiology. 2016). 68(13):1476–88. https://doi.org/10.1016/j.jacc.2016.05.011.


National Health Insurance Service. 2019 national health screening statistical yearbook [internet] Gangwon province. National Health Insurance Service, 2020;[cited 2021 August 29]. Available from:, https://www.hira.or.kr/bbsDummy.do?pgmid=HIRAA020045020000&brdScnBltNo=4&brdBltNo=2312&pageIndex=1
Zaharova S, Litwack K, Gopalakrishnan S, Ellis J, Saltzberg MT. Selfmanagement in heart failure: the importance of self-regulation but not complexity of condition. Western Journal of Nursing Research 2021, in press, https://doi.org/10.1177/0193945921997428


Lim NK, Lee SE, Lee HY, Cho HJ, Choe WS, Kim H, et al. Risk prediction for 30-day heart failurespecific readmission or death after discharge: data from the Korean Acute Heart Failure (KorAHF) registry. Journal of Cardiology. 2019). 73(2):108–13. https://doi.org/10.1016/j.jjcc.2018.07.009.


Youn JC, Han S, Ryu KH. Temporal trends of hospitalized patients with heart failure in Korea. Korean Circulation Journal. 2017). 47(1):16–24. https://doi.org/10.4070/kcj.2016.0429.


Ferreira JP, Kraus S, Mitchell S, Perel P, Piñeiro D, Chioncel O, et al. World Heart Federation roadmap for heart failure. Global Heart. 2019). 14(3):197–214. https://doi.org/10.1016/j.gheart.2019.07.004.


Toukhsati SR, Driscoll A, Hare DL. Patient selfmanagement in chronic heart failure – establishing concordance between guidelines and practice. Cardiac Failure Review. 2015). 1(2):128–31. https://doi.org/10.15420/cfr.2015.1.2.128.



Srisuk N, Cameron J, Ski CF, Thompson DR. Heart failure family-based education: a systematic review. Patient Education and Counseling. 2016). 99(3):326–38. https://doi.org/10.1016/j.pec.2015.10.009.


Liljeroos M, Ågren S, Jaarsma T, Å restedt K, Strö mberg A. Long term follow-up after a randomized integrated educational and psychosocial intervention in patient-partner dyads affected by heart failure. Plos One. 2015). 10(9):1–16. https://doi.org/10.1371/journal.pone.0138058.

Kitko L, McIlvennan CK, Bidwell JT, Dionne-Odom JN, Dunlay SM, Lewis LM, et al. Family caregiving for individuals with heart failure: a scientific statement from the American Heart Association. Circulation. 2020). 141(22):864–78. https://doi.org/10.1161/CIR.0000000000000768.

Chen Y, Zou H, Zhang Y, Fang W, Fan X. Family caregiver contribution to self-care of heart failure: an application of the information-motivationbehavioral skills model. Journal of Cardiovascular Nursing. 2017). 32(6):576–83. https://doi.org/10.1097/JCN.0000000000000398.

Vellone E, Chung ML, Cocchieri A, Rocco G, Alvaro R, Riegel B. Effects of self-care on quality of life in adults with heart failure and their spousal caregivers: testing dyadic dynamics using the actor-partner interdependence model. Journal of Family Nursing. 2014). 20(1):120–41. https://doi.org/10.1177/1074840713510205.


Jonkman NH, Westland H, Groenwold RH, Å gren S, Atienza F, Blue L, et al. Do Selfmanagement interventions work in patients with heart failure? An individual patient data metaanalysis. Circulation. 2016). 133(12):1189–98. https://doi.org/10.1161/CIRCULATIONAHA.115.018006.



Piamjariyakul U, Werkowitch M, Wick J, Russell C, Vacek JL, Smith CE. Caregiver coaching program effect: reducing heart failure patient rehospitalizations and improving caregiver outcomes among African Americans. Heart & Lung. 2015). 44(6):466–73. https://doi.org/10.1016/j.hrtlng.2015.07.007.

Buck HG, Stromberg A, Chung ML, Donovan KA, Harkness K, Howard AM, et al. A systematic review of heart failure dyadic self-care interventions focusing on intervention components, contexts, and outcomes. International Journal of Nursing Studies. 2018). 77, 232–42. https://doi.org/10.1016/j.ijnurstu.2017.10.007.


Cheng HY, Chair SY, Chau JPC. Effectiveness of a strength-oriented psychoeducation on caregiving competence, problem-solving abilities, psychosocial outcomes and physical health among family caregiver of stroke survivors: a randomised controlled trial. International Journal of Nursing Studies. 2018). 87, 84–93. https://doi.org/10.1016/j.ijnurstu.2018.07.005.


Mou H, Wong MS, Chien WT. Effectiveness of dyadic psychoeducational intervention for stroke survivors and family caregivers on functional and psychosocial health: a systematic review and metaanalysis. International Journal of Nursing Studies. 2021). 120, 103969https://doi.org/10.1016/j.ijnurstu.2021.103969.


Cassidy L, Hill L, Fitzsimons D, McGaughey J. The impact of psychoeducational interventions on the outcomes of caregivers of patients with heart failure: a systematic review and metaanalysis. International Journal of Nursing Studies. 2021). 114, 103806https://doi.org/10.1016/j.ijnurstu.2020.103806.


Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and metaanalysis protocols (PRISMA-P) 2015 statement. Systematic Reviews. 2015). 4(1):1–9. https://doi.org/10.1186/2046-4053-4-1.




Higgins JP, Altman DG, G⊘tzsche PC, Jü ni P, Moher D, Oxman AD, et al. Cochrane Statistical Methods Group. The Cochrane collaboration's tool for assessing risk of bias in randomised trials. British Medical Journal. 2011). 343, d5928https://doi.org/10.1136/bmj.d5928.

Borek AJ, Abraham C, Smith JR, Greaves CJ, Tarrant M. A checklist to improve reporting of group-based behaviour-change interventions. BioMed Central Public Health. 2015). 15, 1–11. https://doi.org/10.1186/s12889-015-2300-6.


Å gren S, Evangelista LS, Hjelm C, Strö mberg A. Dyads affected by chronic heart failure: a randomized study evaluating effects of education and psychosocial support to patients with heart failure and their partners. Journal of Cardiac Failure. 2012). 18(5):359–66. https://doi.org/10.1016/j.cardfail.2012.01.014.



Dunbar SB, Clark PC, Reilly CM, Gary RA, Smith A, McCarty F, et al. A trial of family partnership and education interventions in heart failure. Journal of Cardiac Failure. 2013). 19(12):829–41. https://doi.org/10.1016/j.cardfail.2013.10.007.


Å gren S, Berg S, Svedjeholm R, Strö mberg A. Psychoeducational support to post cardiac surgery heart failure patients and their partners-a randomised pilot study. Intensive and Critical Care Nursing. 2015). 31(1):10–8. https://doi.org/10.1016/j.iccn.2014.04.005.

Piette JD, Striplin D, Marinec N, Chen J, Trivedi RB, Aron DC, et al. A mobile health intervention supporting heart failure patients and their informal caregivers: a randomized comparative effectiveness trial. Journal of Medical Internet Research. 2015). 17(6):1–18. https://doi.org/10.2196/jmir.4550.

Vellone E, Chung ML, Alvaro R, Paturzo M, Dellafiore F. The influence of mutuality on self-care in heart failure patients and caregivers: a dyadic analysis. Journal of Family Nursing. 2018). 24(4):563–84. https://doi.org/10.1177/1074840718809484.


Lyons KS, Johnson SH, Lee CS. The role of symptom appraisal, concealment and social support in optimizing dyadic mental health in heart failure. Aging & Mental Health. 2021). 25(4):734–41. https://doi.org/10.1080/13607863.2020.1711866.

Son YJ, Kim SH, Kim SH, Song EK. The influences of cognitive function on adherence to self-care in elderly patients with heart failure. Korean Journal of Health Promotion. 2010). 10(2):61–70.
Cannon JA, Moffitt P, Perez-Moreno AC, Walters MR, Broomfield NM, McMurray JJV, et al. Cognitive impairment and heart failure: systematic review and metaanalysis. Journal of Cardiac Failure. 2017). 23(6):464–75. https://doi.org/10.1016/j.cardfail.2017.04.007.


Son YJ, Shim DK, Seo EK, Won MH. Gender differences in the impact of frailty on 90-day hospital readmission in heart failure patients: a retrospective cohort study. European Journal of Cardiovascular Nursing. 2021). 20(5):485–92. https://doi.org/10.1093/eurjcn/zvaa028.


Strö mberg A, Luttik ML. Burden of caring: risks and consequences imposed on caregivers of those living and dying with advanced heart failure. Current Opinion in Supportive and Palliative Care. 2015). 9(1):26–30. https://doi.org/10.1097/SPC.0000000000000111.


Ok JS, Ko IS, Rhy KH, Kim SH, Lim SJ. Factors affecting to adherence to self-care behaviors among inpatients with heart failure in Korea. Journal of Korean Critical Care Nursing. 2013). 6(2):51–64.
Jo A, Ji SE, Son YJ. The roles of health literacy and social support in improving adherence to self-care behaviours among older adults with heart failure. Nursing Open. 2020). 7(6):2039–46. https://doi.org/10.1002/nop2.599.



- TOOLS
-
METRICS

-
- 1 Crossref
- 3,865 View
- 127 Download
- Related articles in J Korean Crit Care Nurs